Conquer Constipation: Why You’re Backed Up and How to Fix It
Disclaimer: This article contains general medical information. It is not intended to provide any recommendations or advice to a specific individual
and should not be used for this purpose. All readers should discuss their own health care with their primary or specialist physicians or both. The author
disclaims any responsibility for any action, or the results of any action, based on the information provided herein.
We’ve all experienced constipation at some point, but what exactly is it? Most people think of constipation as any kind of trouble having
a bowel movement – either irregularity or pain, or excessive straining when one does occur. A useful working definition of constipation is
having fewer than three bowel movements per week, or bowel movements that are hard, dry, or pellet-like, rendering them painful or difficult to pass.http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/constipation/Pages/definition-facts.aspx
Constipation may also be manifested by a feeling of a blockage in the rectum, or a sense that you cannot fully empty all the stool.http://www.mayoclinic.org/diseases-conditions/constipation/basics/definition/CON-20032773
It is a misconception that good health depends on having a bowel movement every single day.
Anywhere from three times a week to three times a day can be normal.http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/constipation/Pages/definition-facts.aspx It’s all based on the individual and
circumstances. For instance, constipation may affect a person who is travelling or experiencing high levels of stress.
Read on to learn more about constipation, who it affects, and how you can alleviate the slow going.
What Causes Constipation?
Idiopathic Constipation and Irritable Bowel Syndrome
The most common cause of constipation is “unknown,” or to use the medical term, idiopathic constipation. Idiopathic constipation
is closely related to another disorder of unknown cause, irritable bowel syndrome (IBS). IBS is a very common condition associated with recurrent abdominal
pain that begins with a change in stool frequency or form and improves with a bowel movement.http://www.ncbi.nlm.nih.gov/pubmed/16678561 It may be associated with constipation, diarrhea,
or both in an alternating pattern. If your constipation is associated with bloating, crampy pain, intermittent periods of normal stools, pain
that is relieved by a bowel movement, or episodes of loose stools without the use of laxatives, it is probably IBS.
Drugs
Many drugs can cause constipation; check with your doctor to see if any medications you take may contribute to constipation.http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/constipation/Pages/definition-facts.aspx
These are the most common ones that cause constipation:
- Opioids (narcotics): Vicodin, Percocet, Oxy-Contin, and many others
- Blood pressure medications
- Iron
- Antacids containing aluminum
- Sucralfate (Carafate)
- Antihistamines
- Antidepressants
Risk Factors, Diseases, or Conditions
Constipation is more common in women, non-Caucasians, and the elderly.http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/constipation/Pages/definition-facts.aspx
It may run in families. Other risk factors, diseases, and conditions include:http://www.mayoclinic.org/diseases-conditions/constipation/basics/definition/CON-20032773
- Poor diet that includes a lot of processed food and lacks fiber
- Lack of exercise
- Being too busy to go to the bathroom when the need arises
- Pregnancy
- Diabetes mellitus
- Multiple sclerosis
- Spinal cord injury
- Parkinson’s disease
- Decreased thyroid or parathyroid function
- Scleroderma
- Anorexia nervosa
- Gastrointestinal diseases
- Anal fissure
- A tiny tear in the anus that can cause bleeding and severe pain
- Osmotic intestinal obstruction
- A blockage in the small or large intestine that may be partial or complete.http://www.uptodate.com/contents/small-bowel-obstruction-the-basics?source=see_link Food, fluid, and gas cannot pass through, resulting in pain,
vomiting, constipation, diarrhea, and distention. This is usually a critical illness that requires hospitalization.
Underlying causes include adhesions (scar tissue constricting the intestine), tumors, narrowing, twisted bowel, or inflammation.
- Colon or rectal cancer
- Which can slowly progress to partial or complete obstruction
- Bowel disorders associated with inflammation
- Such as Crohn’s disease, ulcerative colitis, and diverticulitis
- Slow transit constipation
- A very long delay in stool moving through the colon, due to weakness in muscles or nerves controlling bowel contractions
- Pelvic floor dysfunction (aka dyssynergic defacation)
- Trouble expelling stool from the rectum due to difficulty relaxing the muscles of the rectum or anus.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2920196/
This is often diagnosed by anorectal manometry, a test done by inserting a probe in the rectum that measures pressure
generated when a person squeezes the anal muscles or bears down to have a bowel movement.
How to Relieve Constipation
Many people prefer to try dietary modifications and over-the-counter medications before seeing a doctor.
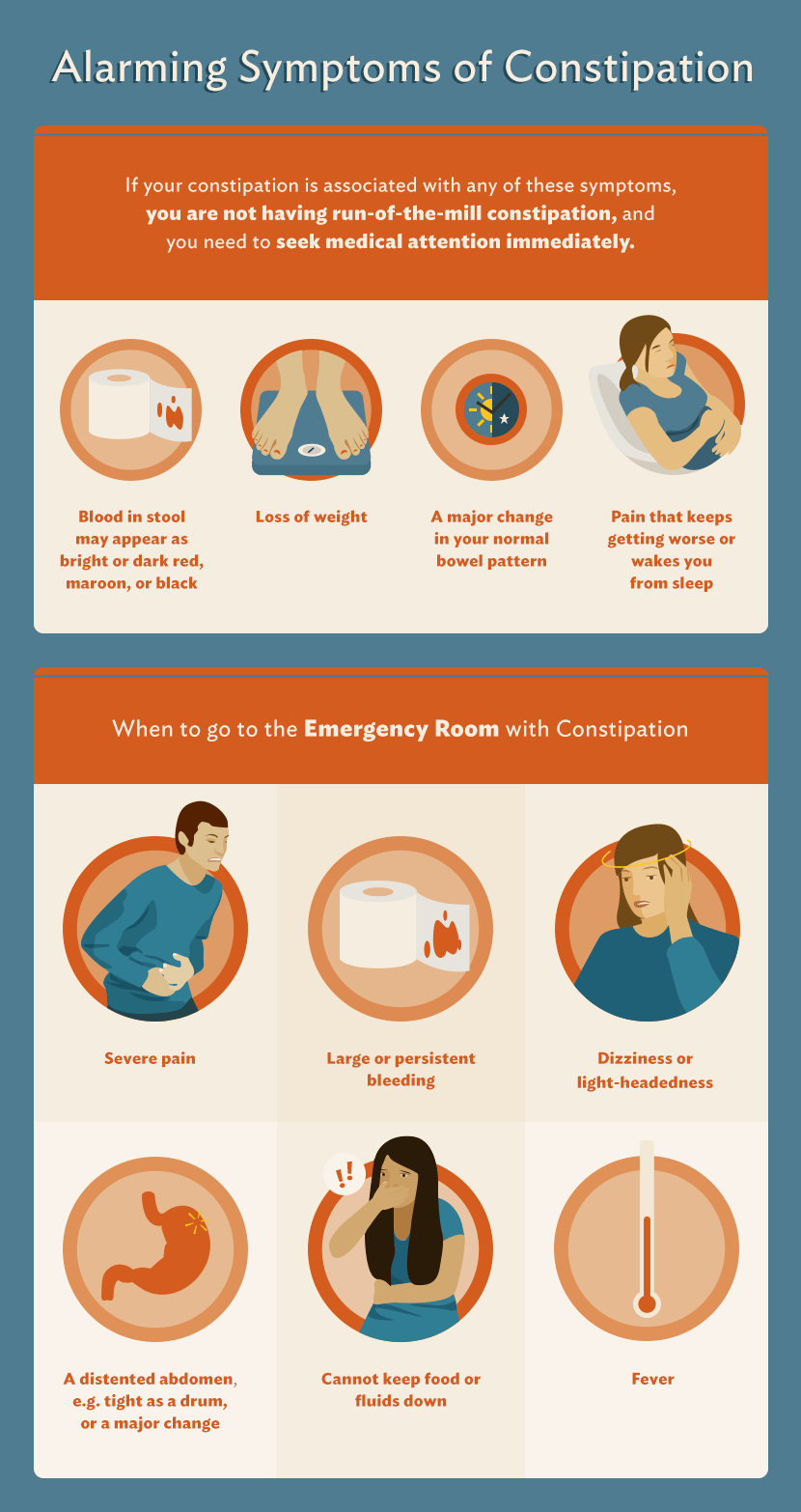
If you have alarming symptoms, or if your constipation gets progressively worse or does not respond to any
treatment, contact your doctor. Here are some tried-and-true approaches to treating constipation:
Treat the Underlying Disease
Diagnosing, treating, and resolving an underlying disease or condition can lead to significant improvement.
Eliminate Drugs that Cause Constipation
Use of multiple drugs to treat various conditions is common. In fact, it’s not uncommon for people to take five or
more drugs that can cause constipation. Review all of your medications with your physician and determine which ones, if any, can be eliminated.
Schedule a Time for a Bowel Movement
Sometimes selecting a time to make the effort to go to the bathroom can allow you to train yourself to go more regularly.
For some, the issue is allocating the time amidst hectic schedules. For others, there may be anxiety due to previous failed attempts.
Try to relax and not pressure yourself. Avoid prolonged sitting and straining if possible. If it doesn’t happen in five minutes, come back later.
Squatting
In Western societies, we have bowel movements while sitting on a raised toilet seat above a bowl. The human body, however,
was designed to do it in a squatting position. Squatting was probably the go-to before the toilet was invented, and continues
to be used by millions of people around the world. So what’s the difference? Squatting straightens the anorectal canal and relaxes the abdominal muscles.https://vw-squattypotty.storage.googleapis.com/uploads/2015/03/03/files/Saeed-Rad.pdfhttp://www.ncbi.nlm.nih.gov/pubmed/26676214
Both can reduce the amount of straining necessary for a bowel movement.http://www.ncbi.nlm.nih.gov/pubmed/?term=sikirov+d Comparative studies of sitting on a toilet bowl versus squatting show the latter is
associated with a greater sense of complete bowel emptying, along with reduced straining.https://vw-squattypotty.storage.googleapis.com/uploads/2015/03/03/files/Saeed-Rad.pdfhttp://www.ncbi.nlm.nih.gov/pubmed/?term=sikirov+d
In countries such as the United States – where raised toilet seats are universal – it
is possible to compensate by placing a small plastic or wooden stool under your feet.
This puts you in more of a squatting position. A commercial product, the Squatty Potty, is available online. It has a raised area on which to
place your feet and it wraps around the base of the toilet.https://www.squattypotty.com/
Exercise
Most people do not get enough exercise, and movement can help stimulate the intestinal tract. Get a good pair of walking or running shoes and ease into
exercise slowly. If you have heart or lung disease or other medical problems, consult your doctor before initiating an exercise regimen.
For a simple walking program, start with five to 10 minutes of slow walking and gradually advance to 15 to 20 minutes of steady,
continuous walking with increasing pace, four to five days per week. Schedule it like a business meeting, and don’t forget it.
If you already exercise, keep it up, but increases in time and intensity are not likely to improve constipation.Enders, Giulia. Gut: The Inside Story of Our Body’s Most Underrated Organ. 2015; Greystone Books, Vancouver, Canada.
Pelvic Floor Therapy
If you have pelvic floor dysfunction, you may benefit from therapy that helps retrain the muscles of the anus and rectum.
This is done using biofeedback, in which a probe is placed in the rectum or vagina to measure pressure. You view the results in
real -time and can work to make modifications with the guidance of a therapist. Suppositories containing a glycerin or a laxative can also help for pelvic floor dysfunction.http://www.webmd.com/digestive-disorders/tc/constipation-age-12-and-older-home-treatment
Increase Fluid Intake
Many of us don’t drink enough fluids, which can contribute to hard, dry stools. Increasing fluid intake through food and drink can make a big difference.
Increase Dietary Fiber
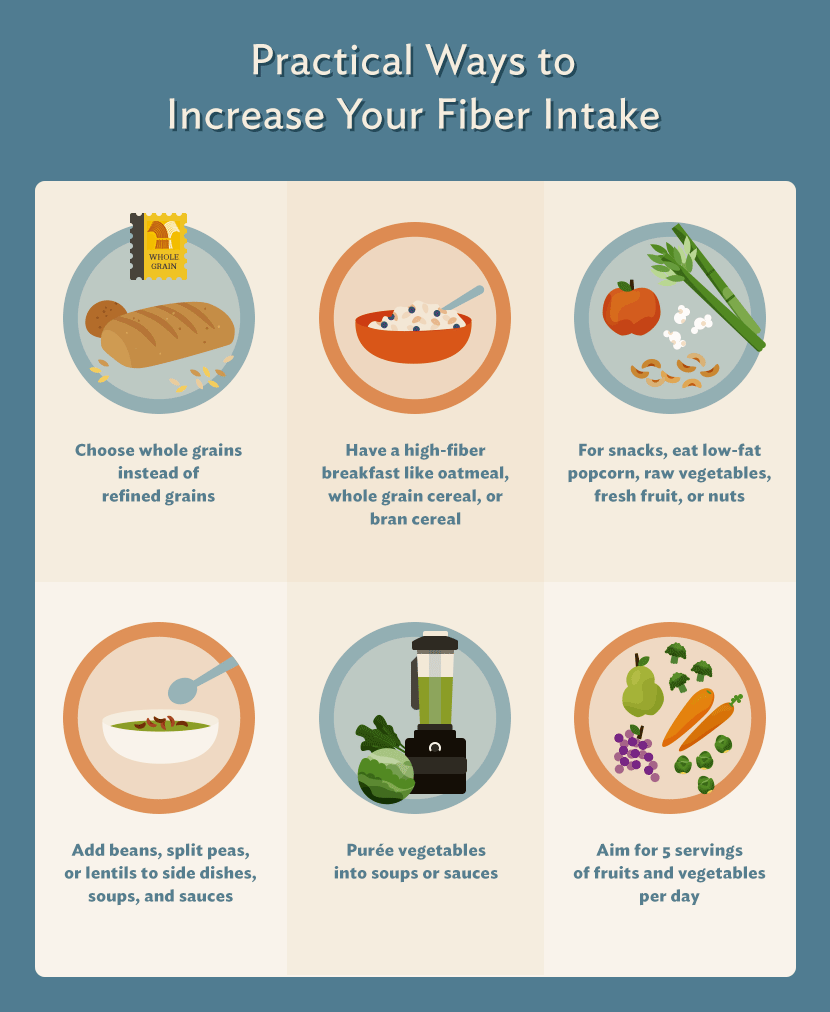
Dietary fiber consists of the elements of plant-derived food that humans cannot digest.http://www.ncbi.nlm.nih.gov/pubmed/18953766
Fiber has several effects that can alleviate constipation: increased stool bulk, increased
stool water consumption, and increased rate of movement through the intestines.http://www.ncbi.nlm.nih.gov/pubmed/23545709 In addition,
the normal bacteria we all have in our stool (collectively known as the microbiome) can ferment
some types of fiber while other varieties are non-fermentable. Both types are potentially beneficial
for constipation, and many plant foods contain them. But keep this in mind: Fermentable fiber can increase gas production.
While fine-tuning your fiber intake by trying specific foods individually may help, the more important goal is to
increase total fiber intake. Most Americans consume only 15 grams of fiber daily. Shoot for these recommended amounts:http://www.ncbi.nlm.nih.gov/pubmed/18953766http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983
- Women
- Adults up to age 50: 25 grams
- Over age 50: 21 grams
- Men
- Adults up to age 50: 38 grams
- Adults over age 50: 30 grams
Dietary fiber is found in fruit, vegetables, legumes (beans, peas, lentils), whole grains, nuts, and seeds.
A high-fiber diet for constipation requires adequate fluid intake, so drink at least eight to 10 glasses of clear
liquid per day. Also, fiber can cause gas and bloating in some people, especially when the constipation is caused
by nervous system problems, like with Parkinsons’s disease or slow-transit constipation. Increasing your fiber intake gradually,
not all at once, can reduce the discomfort fiber sometimes causes. Individual results may vary, and keeping a food and symptom diary can be very helpful.
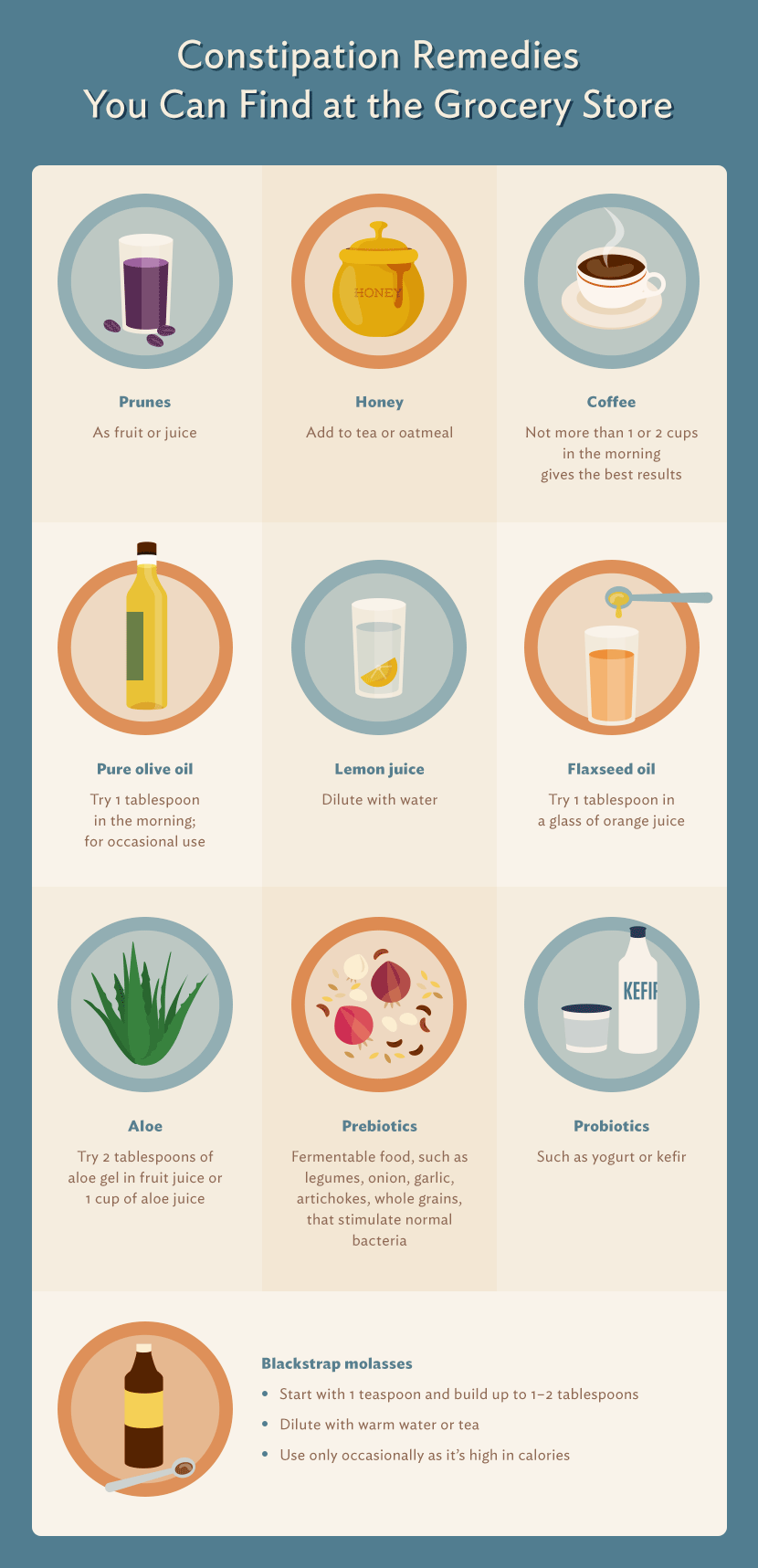
Dietary Remedies
Some foods and drinks, including olive and flaxseed oils, coffee, and honey, have been shown to relieve constipation.
- Laxatives
- Laxatives should never be the first approach for constipation. Start with fiber, fluids, and exercise.
If these and other measures fail, five general types of laxatives are available over the counter:
- Fiber supplements
- These can be combined with a high-fiber diet to augment the beneficial effects noted above.
Examples include: methylcellulose (Citrucil), polycarbophil (FiberCon), and psyllium (Konsyl, Metamucil).
Laxatives containing psyllium or cellulose have the best supporting evidence, but individual results may vary.http://lpi.oregonstate.edu/mic/other-nutrients/fiber
Drinking a large glass of water after each use is advisable.
- Osmotic agents
- These draw fluid into the intestinal tract and keep it there,
causing more and softer stools. Rarely, they can cause dehydration or electrolyte imbalance.http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/constipation/Pages/definition-facts.aspx Examples include: lactulose, milk of magnesia, sorbitol, and polyethylene glycol (MiraLax).
- Stool Softeners
- They pull water and fat into the stool, making it softer.
Take with a large glass of water. Examples include: Docusate (Colace or Surfak).
- Lubricants
- They coat the stool and let it pass more easily. Example: mineral oil
- Stimulant Laxatives
- These irritate the intestines, causing them to contract. Prolonged use may lead to electrolyte imbalance.
They are not the first choice and are best used on an as-needed basis. Examples include: Bisocodyl (Dulcolax or Correctol) and senna (Senokot). Take with a large glass of water.
The three-day rule – taking laxatives every three days rather than daily – may be a fruitful approach.Enders, Giulia. Gut: The Inside Story of Our Body’s Most Underrated Organ. 2015; Greystone Books, Vancouver, Canada.
Normally, only part of the colon empties after a bowel movement, but a strong laxative can clear out the entire colon.
You may not have another stool for the next two days, but if you took laxatives on those days you would falsely conclude that the laxative no longer worked.
- Prescription Medications
- These can be effective if laxatives fail.
- Lubiprostone (Amitiza)
- Draws fluid into the GI tract. Possible side effects include diarrhea, nausea, bloating, and abdominal pain.
- Linaclotide (Linzess)
- Draws fluid into the GI tract and speeds up stool movement. Can cause abdominal pain or diarrhea.
- Naloxegol (Movantik
- Used for constipation caused by opioids. Can cause abdominal pain, diarrhea, nausea, opioid withdrawal, and rarely, bowel perforation.
- Surgery
- Surgery is indicated for cancer and some large polyps of the colon, and in some cases of intestinal obstruction. Very rarely,
removal of the colon is performed for severe, refractory constipation, usually associated with slow-transit constipation.
Prevention of Constipation
Preventing constipation and keeping your gut healthy are even better than treatment. Advances in our knowledge
about gut health accompany increasing recognition of the importance of the microbiome. To keep your gut healthy,
consume enough fiber and fluids, include a variety of high-fiber foods, avoid processed foods, and exercise regularly.
Stress reduction and treatment of depression and other mental disorders – which are diseases, not character flaws – are very important because the brain and gut have many complex interactions.
Embed the article on your site

